Scar Tissue and Nerve Damage: Rehabilitation Considerations
Scar tissue management is essential for effective rehabilitation, especially when nerve damage is involved. Scar tissue forms as the body heals, but it may affect nerve function significantly. Understanding this complex relationship is vital for any rehabilitation program. Both scar tissue and nerve damage can lead to discomfort, restricted movement, and often chronic pain. Physiotherapists and rehabilitation professionals must assess each individual’s situation carefully. Employing techniques that reduce scar tissue can improve nerve function and potentially alleviate pain. Different modalities can be utilized, including manual therapy, ultrasound, and specific exercises. These interventions aim to restore normal mobility. Additionally, educating patients on the importance of this rehabilitation process is crucial. Proper home care techniques play a significant role in recovery. This education enables patients to take an active role in their rehabilitation journey. Involving patients in their recovery process markedly improves outcomes. Long-term positive results may include enhanced quality of life. By addressing both issues concurrently, rehabilitation practitioners maximize recovery potential. Collaboration between healthcare professionals is also essential in fostering comprehensive approaches to scar tissue management and nerve damage recovery.
Understanding Scar Tissue
Scar tissue is a natural part of the healing process following injury or surgery. Over time, it replaces damaged tissue and can be less flexible. This can lead to mobility limitations or associated pain. Nerve damage can occur during this process if the scar tissue affects nearby nerves. It’s important to monitor any symptoms closely. Patients may experience numbness, tingling, or discomfort. Regular assessments by healthcare professionals can help identify these issues early. Rehabilitation programs need to include both the management of scar tissue and the assessment of nerve function. Various tools and techniques can be employed by rehabilitation specialists to help manage these conditions. Manual therapy techniques can assist in breaking up dense scar tissue. Furthermore, specific stretches can facilitate increased mobility and reduce pain. Treatment may also include electrical stimulation for nerve-related issues. Collaborating with medical professionals ensures a more effective rehabilitation strategy. Each patient’s needs are unique and require tailored approaches for effective management. This comprehensive understanding is essential to successful rehabilitation. Practitioners should remain informed about the latest techniques and research in scar tissue management. Staying current enhances treatment options and patient outcomes significantly.
Incorporating a multidisciplinary approach is key to effective rehabilitation. Collaboration among physiotherapists, occupational therapists, and medical doctors ensures all aspects of recovery are addressed. Each professional brings unique insights, strengthening the overall rehabilitation strategy. Physical therapists focus on flexibility and strength training, while occupational therapists concentrate on functional everyday tasks. This teamwork enhances the patient’s rehabilitation experience. Returning to normal activities involves rebuilding strength and increasing mobility in a safe manner. Each discipline requires communication and cooperation. Regular coordination meetings can facilitate this process, ensuring everyone stays informed about the patient’s progress. Pain management strategies must also be integrated, addressing both physical and emotional aspects of recovery. The mental state often influences recovery outcomes and must not be neglected. Well-planned, consistent follow-ups and feedback loops among healthcare providers can optimize results over time. Addressing potential psychological challenges early on, such as anxiety or depression related to injury recovery, is equally vital. Referrals to counselling professionals may also be beneficial for patients needing support. Such comprehensive care increases patient engagement and satisfaction, as well as reducing recovery times. Understanding the connection between physical and mental health can significantly affect rehabilitation success.
Patient education is an important element in rehabilitation and recovery. Educating patients about scar tissue and nerve damage fosters awareness and understanding, encouraging active participation in their recovery. Patients can benefit from understanding the nature of their condition and the rehabilitation processes involved. Informing them about their expected recovery timeline can also reduce anxiety. This knowledge empowers patients to adhere to prescribed rehabilitation programs more willingly. Simple home exercises to manage scar tissue can be taught during sessions. Patients often respond positively when they take responsibility for their healing journey. Demonstrating stretches and mobility exercises at home promotes continuous improvement. This approach also ensures they remain engaged throughout the process. Regular check-ins with rehabilitation professionals help consolidate learning and adjustment of programs to their evolving needs. Encouraging open dialogue about challenges fosters trust and builds rapport between patients and healthcare providers. As a result, adherence to the rehabilitation plan improves significantly. An informed patient is more likely to achieve better health outcomes. When patients feel empowered, they tend to maintain motivation, which is essential for long-term success. Creating a supportive atmosphere encourages them to seek guidance anytime challenges arise during their rehabilitation journey.
Techniques for Effective Scar Tissue Management
Scar tissue management can significantly influence the function of affected areas. Various therapeutic approaches exist to manage scar tissue effectively. Among them are manual therapy, stretching, and specific exercises, which should all be tailored to the individual’s needs. Manual therapy techniques can include myofascial release or cross-fiber massage. These methods aim to improve blood circulation and tissue flexibility, minimizing restrictions. Stretching exercises can significantly contribute to scar tissue reduction and improved range of motion. Therapeutic exercises strengthen the surrounding muscles, promoting better support for the affected areas. Implementing these techniques requires proper training and knowledge to ensure safety and effectiveness. Physiotherapists should provide patients with guidance on how to perform these exercises correctly. Additionally, educating patients about optimal positioning during activities fosters better rehabilitation outcomes. Regular monitoring and modification of therapy plans ensure tailored approaches based on patient responses. This adaptability maximizes recovery potential. Pain management strategies, such as ice application or topical treatments, can further aid the rehabilitation process. Combining different techniques creates a holistic approach towards proper scar tissue management. This comprehensive strategy can lead to improved functional outcomes while minimizing the risk of complications.
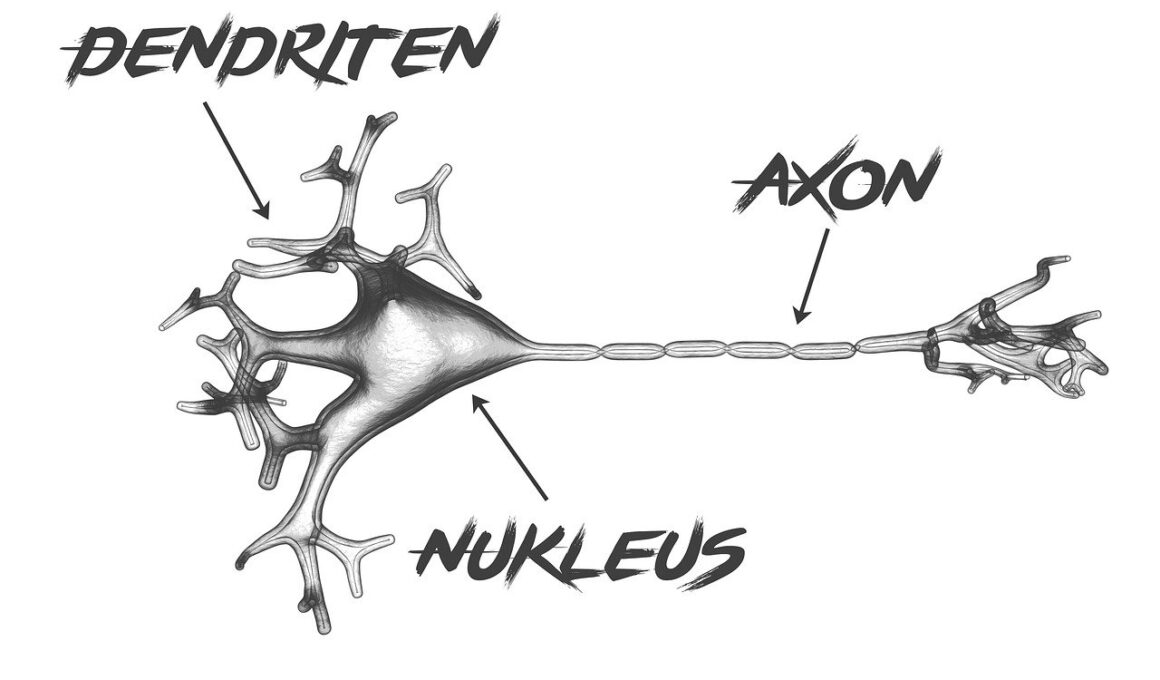
Understanding the impact of scar tissue on nerve function is crucial for rehabilitation. Scar tissue can invade and compress nerves, resulting in pain or dysfunction. This pressure alters the normal patterns of transmission, leading to long-term consequences. Patients are often unaware of how these changes affect them over time. Detecting these issues early through assessment is vital for minimizing complications. Healthcare professionals must perform regular neurological examinations. Identifying symptoms such as altered sensation or muscle weakness should prompt immediate intervention. Rehabilitation experts can employ tailored interventions, focusing on both scar tissue reduction and nerve restoration. Early intervention often leads to better outcomes and less chronic disability. Regular follow-ups ensure that patients receive appropriate care and timely modifications. Employing modalities such as electrical stimulation may help alleviate nerve-related symptoms. Educating patients about the importance of this monitoring fosters a sense of ownership and participation. This proactive approach empowers them to communicate any concerns arising during rehabilitation. Building awareness about the potential long-term effects of untreated nerve compression is essential. Patients should understand that managing both scar tissue and nerve function can greatly enhance their quality of life. Ensuring well-rounded approaches is essential during their recovery process.
Creating a Long-Term Rehabilitation Plan
Establishing a long-term rehabilitation plan is crucial for effective recovery from scar tissue and nerve damage. Rehabilitation programs should encompass a range of strategies tailored to the individual’s specific needs. Setting realistic goals and timelines provides motivation. Clinicians should assess the patient’s progress regularly, adjusting goals as needed to ensure continuous improvement. Integrating functional activities into the rehabilitation program cultivates better outcomes. Patients need to regain both strength and flexibility for comprehensive recovery. Incorporating exercises that mimic daily tasks enhances the program’s relevance. Aerobic exercises, in addition to strength training, should also be considered for overall physical health. Additionally, a multidisciplinary approach continues to play a vital role in creating effective long-term plans. Engaging professionals, such as dietitians and psychologists, promotes holistic recovery. Healthy nutrition supports the healing process, while addressing mental health challenges can minimize barriers to recovery. Regular communication between team members ensures a unified approach to treatment. This collaboration enhances accountability and helps patients remain motivated. A thoughtfully designed rehabilitation plan aims to facilitate recovery gradually and sustainably. Emphasizing maintenance strategies is crucial for preventing future complications. Encouraging patients to incorporate these techniques into their lifestyle sets the foundation for success.
Final considerations involve addressing ongoing patient support and mentoring. Rehabilitation shouldn’t cease after initial goals are met. Continuous support maintains motivation and enables long-term management of scar tissue and nerve issues. Regular check-ins post-rehabilitation bolster patient confidence. During these sessions, healthcare providers can revisit self-care strategies that patients learned during their rehabilitation. It also allows for adjustments to be made if new issues arise. Providing patients with resources enables them to stay informed about developments in rehabilitation techniques. This ongoing learning fosters a proactive attitude toward their health. Sharing techniques for preventing recurrence should also be emphasized. Patients are often more engaged in their recovery when they feel supported. Offering workshops or group sessions further enhances community among patients. peer support can also be beneficial. Establishing forums where they can share experiences encourages ongoing communication. Such collaborations can lead to improved recovery experiences. In addition, creating a follow-up schedule encourages responsibility for health. Long-term management requires patience and commitment. Supporting patients in their journey fosters resilience, thus enhancing their ability to cope with future challenges. Ultimately, promoting self-management strategies ensures a smoother transition into life post-rehabilitation, creating a stronger foundation for overall well-being.