Cardiovascular Responses to Exercise in Patients with Autonomic Neuropathy
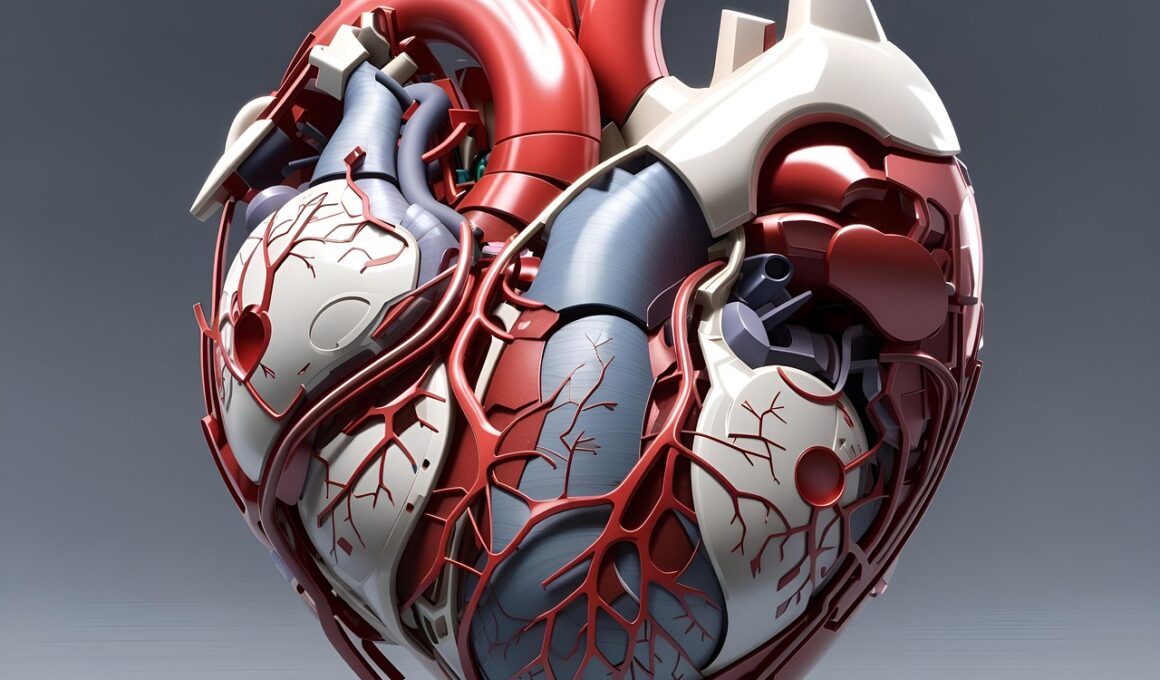
Autonomic neuropathy significantly impacts cardiovascular health by altering heart rate responses during physical activity. Patients with this disorder experience abnormal cardiovascular reflexes, which can lead to inadequate response in heart rate, blood pressure, and overall blood flow. As a result, understanding these unique responses during exercise is essential to design effective rehabilitation strategies. One challenge in assessing these patients lies in the variability of symptoms they experience, which can range from dizziness to fatigue. For rehabilitation professionals, ensuring safety while promoting cardiovascular fitness for these individuals is pivotal. This necessitates a comprehensive approach that considers the individual’s limitations and capabilities. Regular cardiovascular assessment, alongside careful monitoring, becomes imperative to help maintain appropriate responses for those affected. Based on existing knowledge, structured exercise interventions are found to enhance various aspects of cardiovascular functioning. Moreover, awareness of potential complications helps mitigate associated risks during exercise programs. The ultimate aim is to improve the quality of life for patients while also addressing their unique health challenges effectively. This article discusses the physiological mechanisms at play and how tailored exercise programs can support cardiovascular health.
Continued efforts in research underscore the importance of analyzing cardiovascular responses specific to exercise in autonomic neuropathy patients. Assessment techniques can include heart rate variability testing, blood pressure monitoring, and exercise tolerance tests. Doctors and exercise physiologists may find it critical to evaluating baseline functionality before initiating an exercise regime. By focusing on stress responses during exercise, insights into how patients adapt are gained, thus guiding clinical applications promptly. Studies indicate that low to moderate continuous exercise can promote safe adaptations within the cardiovascular system. Meanwhile, high-intensity activities, particularly in prone individuals, may induce adverse events. Therefore, individuals are generally recommended to engage in a gradual increase in activity levels. A tailored approach can involve various modalities such as walking, stationary cycling, and aquatic exercises. Each setting provides a unique benefit while minimizing risks. Supervision through skilled professionals can ensure safety while promoting motivation. Furthermore, education about the potential for self-monitoring heart rate and recognizing symptoms of over-exertion serves to empower patients. Such strategies combined can yield positive long-term outcomes and reduce the prevalence of exercise-related complications in these patients.
Physiological Mechanisms of Exercise
Understanding the physiological mechanisms behind exercise in the context of autonomic neuropathy is critical. The autonomic nervous system plays an essential role in regulating heart rate and vascular responses during physical activity. In patients with autonomic neuropathy, these systems may misfire, resulting in dysautonomia characterized by significant variation in heart function. This disarray can manifest as either excessive tachycardia or bradycardia in response to exercise. Additionally, blood pressure may fluctuate unpredictably. Strenuous physical activity often leads to impaired perception of exertion, possibly causing patients to overexert themselves unknowingly. Such risks necessitate a comprehensive evaluation of the cardiovascular profile and real-time adjustments during exercise. Training can elicit adaptations in the cardiovascular system, facilitating more effective responses over time. Regular exercise has been associated with improved parasympathetic dominance following training adaptations. This can lead to improved heart rate adaptability and reduced cardiovascular risk factors. Understanding and addressing these mechanisms can help guide the rehabilitation process and empower patients in making informed choices while exercising, potentially regenerating their cardiovascular resilience.
Personalized exercise prescriptions can vary greatly, ranging from the frequency of activity to intensities recommended. Drawing on specific patient profiles can lead to more significant outcomes. Key factors to consider include a patient’s age, overall health condition, mobility levels, and any additional comorbidities present. Moreover, a thorough understanding of the intricacies of autonomic dysfunction becomes vital for both healthcare professionals and patients. A collaborative approach will enhance program adherence, facilitating a smoother journey towards achieving fitness goals. The impact of psychosocial factors should also be acknowledged, as mental health greatly influences motivation and exercise behavior. Integrating behavioral counseling may improve overall adherence outcomes. Empowering patients through education highlights how lifestyle choices, such as nutrition and sleep, play equal parts in overall well-being and exercise performance. Additionally, group exercise programs can leverage social support, fostering community and improving motivation levels. Such interventions have shown promise in enhancing the quality of life for individuals with autonomic neuropathy. Ongoing evaluations help maintain and adapt exercise routines to ensure continual progress towards individual health goals, paving the way toward enhanced cardiovascular fitness and patient empowerment.
Exploring Challenges and Solutions
Patients with autonomic neuropathy face unique challenges that require tailored solutions focused on cardiovascular responses. These challenges may include orthostatic hypotension, inadequate blood flow, and unexpected cardiovascular drift, particularly during prolonged exercise. As a result, regular monitoring of vital signs is essential to navigate these challenges safely. Healthcare professionals must remain vigilant regarding symptom recognition, ensuring that any significant changes in heart rate or blood pressure are caught early. To address potential adverse effects, introducing rest breaks within sessions is often beneficial. Moreover, education regarding recognized signs of fatigue or distress equips patients with necessary health literacy. Implementing phase-based progression and incorporating flexibility in exercise routines allows the incorporation of individual capabilities into their plans. Use of wearable technology can also aid in real-time monitoring of physiological responses, providing valuable data points. Regular feedback helps in making informed adjustments, promoting safety and comfort. Overall, creating a supportive environment fosters not only physical strength but also psychological resilience. In conclusion, addressing these challenges through a multifaceted approach enhances the potential for successful exercise outcomes, making a significant difference in the lives of patients.
Another key aspect influencing cardiovascular responses during exercise in patients with autonomic neuropathy involves environmental factors. Heat and dehydration can impose significant barriers to safe exercise, particularly for those already facing autonomic dysfunction. Providers must educate patients on the importance of hydration and acclimatization strategies prior to engagement in an exercise program. Optimal conditions, such as temperature regulation and safe environments for activity (e.g., shade, cool water), can greatly affect exercise accessibility. Additionally, understanding individual tolerance levels to environmental factors is critical for ensuring safety during physical exertion. Patients may need to adapt chosen activities to allow for variations in personal comfort and fitness levels. Group exercise settings can also be adjusted to accommodate the necessary modifications while simultaneously fostering social support. Furthermore, recommendations for appropriate clothing and accessories can enhance performance, aiding in better circulation and comfort during activities. Physicians and exercise physiologists, in collaboration with patients, must outline clear guidelines regarding these environmental considerations, further promoting a comprehensive understanding of how to harness positive cardiovascular responses. Supporting these adaptations can enhance overall outcomes.
Future Directions in Research
Research into cardiovascular responses to exercise in patients with autonomic neuropathy continues to evolve, shedding light on both challenges and potential interventions. Future studies can benefit from evaluating specific exercise modalities that might yield the most beneficial cardiovascular adaptations for these patients. An understanding of how individual genetic and environmental factors impact response to exercise encourages a personalized approach to rehabilitation efforts. Analyzing biomarkers associated with autonomic function may unveil new avenues for intervention. Promoting research focusing on longitudinal outcomes post-exercise interventions can illustrate the long-term benefits of structured programs for cardiovascular health. Additionally, implementing technological advances such as remote monitoring systems showcases promising applications for optimizing patient care and enhancing rehabilitation protocols. As healthcare systems increasingly prioritize patient-centered care, incorporating feedback from patients regarding accessibility and preferences will become crucial for intervention design. This shift can guide healthcare providers in creating sustainable exercise programs that align with individual lifestyles and preferences. Emerging findings from interdisciplinary research can forge pathways to advancements in treatment strategies, applying evidence-informed exercises designed to enhance cardiovascular responses, optimize functional capacity, and ultimately improve patient quality of life.
In summary, understanding cardiovascular responses to exercise in patients with autonomic neuropathy remains a vital area of research. By implementing tailored exercise protocols, professionals can address the complexities associated with autonomic dysfunction while promoting improved health outcomes. Moreover, enhancing patient education empowers individuals to take control of their exercise regimens, ensuring safety and efficacy at each stage of the rehabilitation process. Through collaborative efforts combining healthcare expertise and patient input, achieving optimal cardiovascular adaptations becomes more feasible. Developing supportive exercise communities further enables individuals with autonomic neuropathy to navigate challenges while inspiring motivation and accountability. Ultimately, the goal remains focused on improving the quality of life while enhancing cardiovascular health in these patients, leveraging established evidence-based practices. As research advances and new discoveries emerge, adaptations in the approach to exercises and patient management will follow, promising a brighter future for individuals facing autonomic neuropathy. Through empowered communities and informed approaches, individuals can build resilience against the challenges posed by their condition, harnessing the potential for improved cardiovascular functioning and overall well-being for a healthier future.